When Tzameret Fuerst wakes up every morning, she has one thing on her mind: Saving 4 million lives through circumcision. Fuerst is the CEO of Circ MedTech, which developed a device to facilitate non-surgical adult male circumcision—a tool that could revolutionize the fight against the spread of HIV.
In 2007, the World Health Organization found that male circumcision can reduce the risk of HIV infection from women to men by about 60 percent [PDF]. The organization concluded that if 80 percent of males in 14 countries were circumcised by 2015, about 4 million HIV infections could be averted and $20 billion saved.
WHO and UNAIDS urged countries to expand access to medical male circumcision, prioritizing countries in sub-Saharan Africa with high HIV prevalence and low levels of circumcision. “This is the equivalent of a 60 percent effective vaccine for men… It’s clearly the most obvious, most cost-effective intervention we could use to dramatically change the course of H.I.V. in the near future,” Dr. Stefano Bertozzi, director of H.I.V. and tuberculosis for the Bill and Melinda Gates Foundation told The New York Times in September.
But so far, only 5 percent of the WHO goal has been reached, the majority in Kenya. Malawi and Rwanda have only reached 0.1 percent of their goal, according to a 2011 WHO report. Scale-up has been “modest,” WHO official Julia Samuelson acknowledges.
There have been major barriers to the campaign. One problem has been the lack of trained medical professionals to carry out surgical circumcision. For example, Malawi, which has an 11 percent HIV rate, has just two doctors for every 100,000 people. Some governments, like Uganda’s, have not been on board. And not all men are willing to undergo a procedure that involves, as Fuerst says, “needles, blood, and a sensitive organ.” (Let’s not forget the scalpel.)
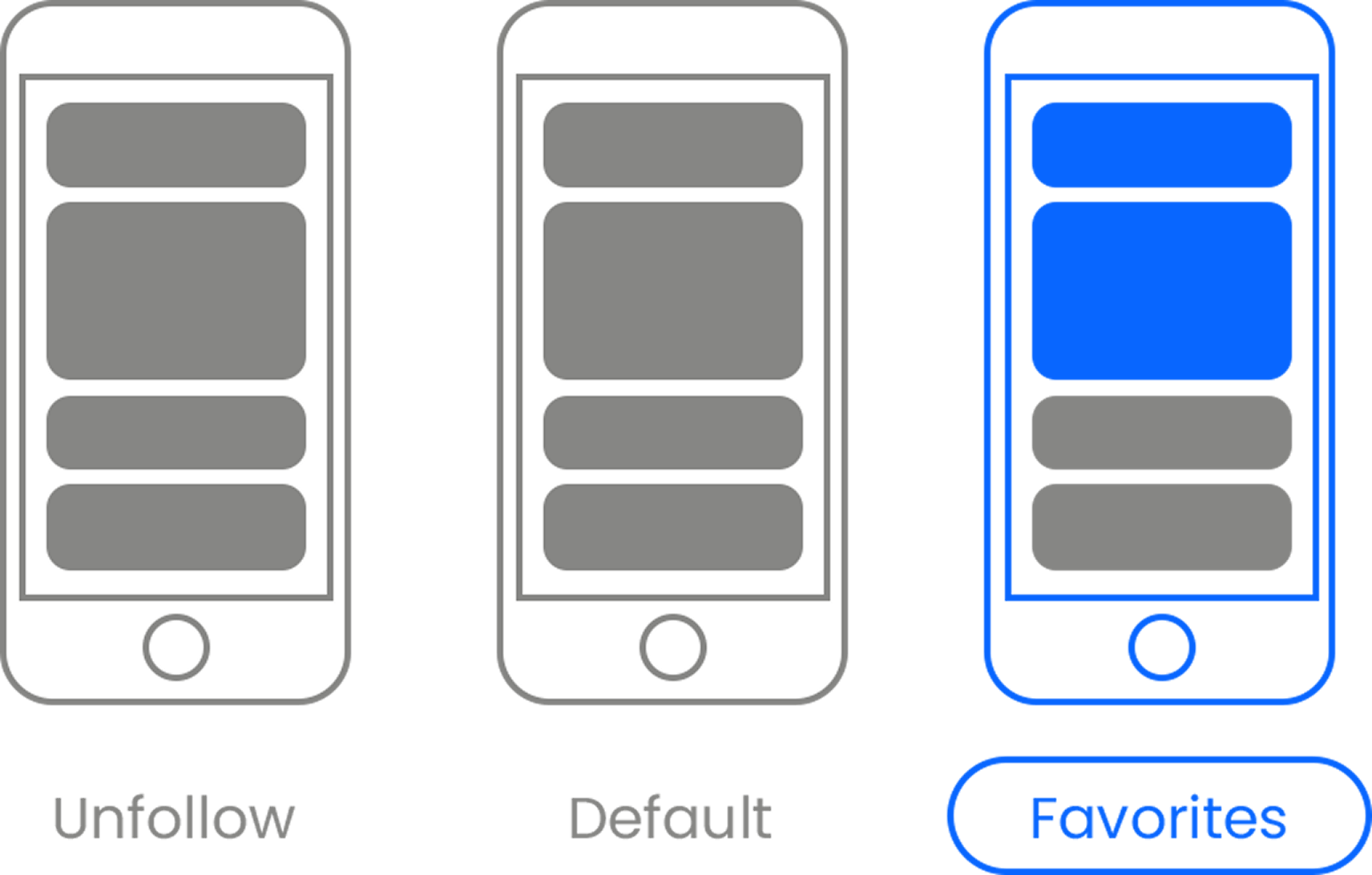
Enter PrePex, a simple device that consists of three rings: two plastic, one elastic. The innovation, which is patent pending, allows for a “virtually painless” adult male circumcision that can be performed by low-cadre nurses almost anywhere. It takes one and a half minutes to place the rings, and the same amount of time to remove them a week later, according to the company’s website. The device stops the flow of blood to the foreskin tissue, which after a week becomes “like fingernails,” and is removed with blunt, safe scissors. (When men return for their second visit, they must also undergo counseling on HIV prevention.) “PrePex marks a revolution in the framework of accelerating HIV prevention,” UNAIDS Executive Director Michael Michel Sidibe says.
The lack of surgery is bound to improve demand, says Fuerst, who has a background in marketing. “One message is come get circumcised—the procedure entails injected anesthesia, bleeding, a surgical procedure and post-healing time,” she says, “versus telling a man: ‘You’re going to go through something that is virtually painless, there’s no blood, there are no needles, and you can go back to work.’ Now think of the impact on uptake.”
Assuming CircMed Tech gets its patent for PrePex, the device will join the cadre of other trademarked innovations for fighting poverty, like Plumpy Nut, a fortified paste for treating children with malnutrition, and the Life Straw, a water filter. There is controversy around using patents for life-saving innovations, however.
“Patents don’t look like a particularly good way to solve the innovation incentive for humanitarian life-saving products for poor countries,” says Owen Barder, a senior fellow at the Center for Global Development. When you receive a patent for a life-saving product you are faced with an ethical problem: “You have to sue people for making life-saving products," he says.
Barder says we need a different way to incentivize innovation for such critical products, like prizes or patent buyouts, for example. But for now, patents are the system we have. “Innovation costs money and grant cycles to nonprofits are typically very long. It would have taken us double the time to get where we are now,” says Fuerst. “By taking a more risky entrepreneurial path, we will ultimately help Africa achieve its goals more efficiently. That is our incentive—the faster we move, the more lives we save.”
“As a social enterprise, we have taken upon us to strike a balance between making a profit and being socially responsible,” she says, noting that her company’s largest investor is the nonprofit Acumen Fund. Still, Fuerst indicated that her company intends into protect its intellectual property. She wouldn’t share the price of the device, saying, “that’s to be negotiated with governments but we are committed to an affordable price.”
No country has bought the PrePex device yet, but Rwanda has approved it after clinical trials, and Zimbabwe has begun testing. In December, Rwanda’s health minister, international HIV expert Agnes Binagwaho, praised PrePex in a Washington Post op/ed, writing that, while not a silver bullet, the device can “revolutionize our [HIV] prevention toolkit in Africa.”
Rwanda’s national goal is to decrease new infections of HIV by 50 percent for boys ages 10 to 19 and 30 percent among men age 20 and older, which would take “more than 12 years” if Rwanda used conventional surgical procedures for circumcision. “We need to reach 2 million men in two years to benefit from the protective effect of the procedure in order to achieve this as part of a comprehensive, combination HIV prevention strategy,” Binagwaho wrote.
“We’re talking about a rate of 4,000 a day. And with PrePex that vision can become a reality,” Fuerst says.
Yet this conveyor-belt vision may not jive with reality. Technology is just one piece of the puzzle. “While devices will likely address some of the implementation challenges, essential ingredients to increasing the pace of scale-up will remain important regardless of the procedure used,” WHO official Julia Samuelson says. If governments aren’t on board, and the value of male circumcision isn’t marketed well, the goal of circumcising 20 million men by 2015 cannot become a reality.
Still, the new technology addresses many of the barriers that have made the program so difficult. “Today we have the only device in the world that we are aware of that can conduct nonsurgical adult male circumcision. And that is a huge value proposition,” Fuerst says.
This is the fourth story in our series on social enterprise in Africa by Laura Burke, a reporter based in Cote d'Ivoire.
Photo via (cc) Flickr user USAID_Images











 Otis knew before they did.
Otis knew before they did.